Contact and Additional Information to be addressed to: Brandon Brown,
653 E. Peltason Drive, AIRB, Rm. 2024,
Irvine, CA 92697-3957.
(949) 824-6996 phone
(949) 824-0529 fax
brandon.brown(at)uci.edu
The 16th century marked the beginning of the fight against sexually transmitted infections (STIs) with the use of the male condom. However, many puzzling questions and prospective solutions have surfaced over the years in the context of condom use. In 1978, a condom riddle introduced the dilemma of a man having two condoms to use for intercourse with three consecutive women. In this paper, we will discuss the solution proposed to the aforementioned riddle, and examine its public health implications. Moreover, we illustrate the challenges involved in condom use and reduction of STI acquisition.
A male condom is a thin sheath worn over a the penis during sexual intercourse to reduce the risk of acquirement and transmission of Human Immunodeficiency Virus (HIV), Sexually Transmitted Infections (STIs), and to prevent pregnancy. Since its first appearance in the 16th century, the male condom, has evolved and as current paradigms suggest, using them consistently and correctly provides protection against the aforementioned conditions (World Health Organization, 2010).
Today, condom availability and use continue to be widespread, especially in developed parts of the world, and play a significant role in public health interventions and outreach efforts, as HIV and other STIs continue to burden communities and societies (Moran et al., 1990). This paper aims to critically examine the “condom riddle”, initially proposed in 1978, and provide alternative solutions with existing paradigms in order to promote safe sexual practices through condom use.
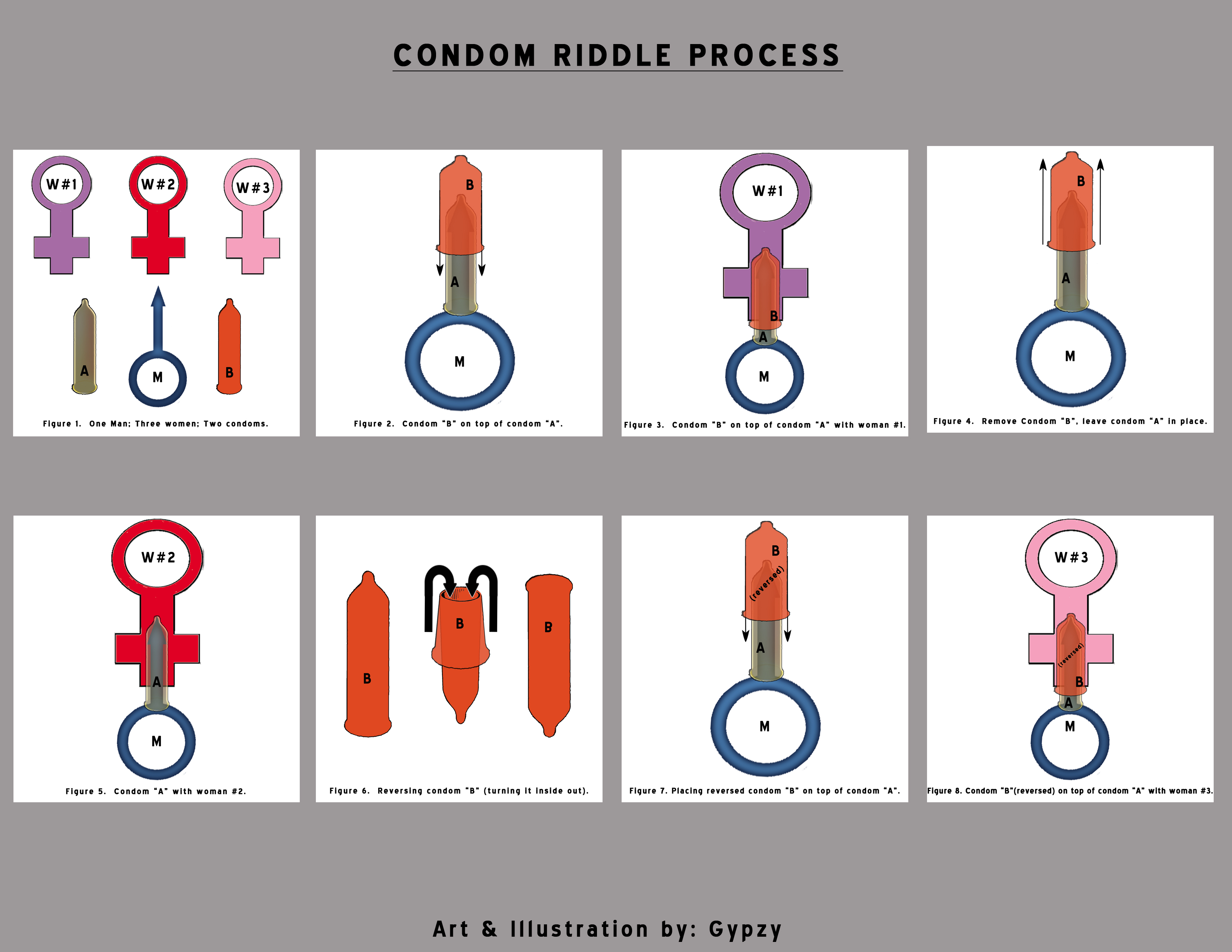
The condom riddle first appeared in an article entitled “An Algorithm prevents the Propagation of Certain Diseases at Minimum Cost”. It was published in 1978 in conference proceedings appropriately titled “Interfaces Between Computer Science and Operations Research”( Lenstra, Rinnooy Kan, & van Emde Boas, 1978). The challenge in the riddle is as follows: If a man were to have sexual intercourse with three women consecutively, but only has two condoms, how would he do so without exposing himself or any of the women to diseases. Dr. Ilan Vardi, a Professor of Computational and Applied Mathematics at Stanford University, proposed a mathematical solution to the problem and published it in his book “Computational Recreations in Mathematica” in 1991(Vardi, 1991). His solution was later translated into a non-mathematical module (Vardi, 1993). The proposed and universal solution to this riddle is as follows: The man in question uses condom “A” and “B” at the same time to have sexual intercourse with woman #1. Then, he takes off condom “B” to have sexual intercourse with woman #2 using condom “A” only. Finally, the man turns condom “B” inside out and places it back on top of condom “A” to have sexual intercourse with woman #3. Through this process, he has sexual intercourse with all three women with two condoms and reduces the risk of exposing himself and the women to STIs as the exchange of bodily fluids is theoretically less. To facilitate understanding of this process, we have provided an illustration of the solution (Figure 1), which has been discussed at length on message boards, blogs, forums, personal websites, books, and University websites (OCF, 2004).
The condom riddle may not be as unrealistic as many would think. A study of sexual behaviors in Puerto Rico identified a 2% self-reported prevalence of group sex activities, with this group possibly more vulnerable to the acquisition and transmission of HIV and STIs (Ortize et al., 2011). The current solution for the riddle does not provide the most effective and safe method of reducing the spread of infection among the four sexually active individuals. In this section, we examine some of the problems associated with the proposed solution from a public health perspective.
Condoms Are Not One-Hundred Percent Effective
As with any form of protection, condoms are not 100% effective. An observational study carried out in the southern United States showed that used condoms ripped during intercourse for 3% of participants, and the rate of a condom ripping was found to be higher for first time users (Hollander, 2005). Other studies indicate that slippage and condom ripping during use may range from 1.0% to 3.6%( Fitch, Stine, Hager, Mann, Adam, & McIlhaney, 2002). Thus, a condom cannot be regarded as a flawless method of reducing the risk of acquisition and transmission of STIs and pregnancy prevention. The solution to the riddle, therefore, does not account for the margin of error in ripping, breakage, and other mechanical problems.
Using Condom A and B Together
In order for condoms to be effective, they must be used correctly. Utilizing the same condom for more than one episode of intercourse, using two or more condoms simultaneously, or wearing a condom inside out presents problems when trying to minimize exposure to bodily fluids. First, a condom must never be used more than once, since this increases the chances of ripping (“What care should be taken to ensure correct male condom use?” 2013). Second, using more than one condom at a time, a practice called “double-bagging”, can lead to increased friction thereby elevating the likelihood of ripping (“Condoms,” 2013). Third, using a condom inside out makes it difficult for a man to remove it after sexual intercourse, leading to an increased risk of exposure to bodily fluids (Hollander, 2005). Therefore, the solution proposed to the riddle fails to account for issues that surface with improper condom use.
Skin-to-Skin Infection
Condoms are not 100% effective in reducing the risk of STI transmission that may occur in areas of the skin that are not protected by the condom (Male Latex Condom: Specification, Prequalification and Guidelines for Procurement, 2010). Genital ulcer diseases such as genital herpes, syphilis and cancroid are examples of such STIs. Furthermore, HPV may also be transmitted from infected skin and lesions not covered by condoms, and lead to genital warts or cancer (Fitch, Stine, Hager, Mann, Adam, & McIlhaney, 2002). Consequently, the riddle solution fails to recognize that STIs vary greatly in their location and ability to spread. If any individual were to be a carrier of an STI transmitted through areas not covered by a condom, all others will be at an increased risk for infection.
STI Testing
Before all four individuals decide to engage in sexual intercourse, it should be recommended that they undergo STI testing. Screening for common STIs such as Gonorrhea and Chlamydia entail a simple urine test. Herpes, HIV, and Syphilis can be detected by serological testing to determine presence of antibodies, and HIV testing is now less invasive with oral swab testing. Trichomoniasis and HPV screening involve a pelvic exam followed by microscopic visualization of genital specimens (Greenwald, Burstein, Pincus, and Branson, 2006) . Furthermore, it is important for these individuals to get tested regularly as STIs have different incubation periods before symptoms appear and some are asymptomatic altogether, constituting a particular challenge. While STI testing is now available in most countries, there are structural and societal barriers to access for economically disadvantaged groups and those living in the developing world (Kolman et al., 2011; Packel, 2012). It is important to note that although STI testing is an important step towards achieving favorable health outcomes, each test carries diagnostic limitations, some STIs are untreatable and correct diagnoses and disease management will depend on the natural history of the disease in question.
Reducing the Number of Lifetime Partners
Abstinence is the ideal method for preventing STIs, but may not be a realistic solution due to societal standards. Fortunately, reducing the number of lifetime sexual partners greatly reduces the acquisition of STIs ( Fitch, Stine, Hager, Mann, Adam, & McIlhaney, 2002). Thus, the solution to the riddle needs to be modified to include a risk analysis of having sexual intercourse with multiple partners in a short period of time. If the man were to just have sexual intercourse with one woman, his and her risk of acquiring STIs would be significantly reduced. However, it is important to note that having sex with one partner does not eliminate the risk of contracting an STI because the partner in question may be infected with an STI and may have varying levels of sexual experience that can significantly increase one’s risk. It is therefore in the best interest of involved parties to engage in open, honest, and consistent dialogue about sexual behaviors and histories, in order protect one another from venereal diseases.
Alternative condoms
For individuals with allergies to latex, non-latex condoms are widely available. Polyurethane condoms are undoubtedly the best alternative. In fact, studies indicate that polyurethane condoms are comparable to latex condom in that they do not have excessively high rates of slippage and breakage, and can be considered a safe-sex method ((Potter & de Villemeur, 2003) . Additionally, study results indicate that other non-latex condoms such as those from polyisoprene (approved by the FDA in 2008), exhibit strong comparability to latex condoms in terms of protection and durability (“Durex Synthetic Polyisoprene Male Condom,” 2008). Lambskin condoms, while effective in preventing pregnancy, are not effective in reducing the likelihood of contracting STIs because of their porous nature and should not be used for that purpose (“Condoms: Barriers of Bad News,” 2009). The evolution of the condom has not ceased with latex and non-latex options. A new innovative form of barrier protection called the Origami condom has gained popularity and is expected to reach the market soon. They are being referred to as the 21st century condom (“About the condoms,” 2013). The male and female Origami condoms provide users with pleasure-oriented silicone without having problems associated with rolling the condom on. The goal of Origami condoms is to increase consumer use, while maintaining sexual pleasure. Female condoms are also an effective tool to reduce the transmission of HIV and STIs. Studies have found reductions in the prevalence of STIs among women who engaged in sexual intercourse where both a female and male condom was present (Fontanet et al., 1998; Macaluso, 2000).
However, condoms of all types and materials have the disadvantage of not covering the entire genital area, leaving skin vulnerable to exposure to particular STIs. To address the surface area limitation of traditional condoms, we recommend a new condom design that would cover a larger portion of the genitalia. The proposed condom design would cover the testicles in order to reduce the risk of STIs that may be contracted from bodily fluids and skin-to-skin contact. More research is needed to examine the acceptability of such a condom.
Education
Another important component in addressing the posted condom riddle solution is education focused on proper condom use (D’Anna, 2012). As studies have shown, incorrect practices such as not withdrawing the penis after ejaculation, improper holding of the condom as it is placed on the penis, not pinching the tip of the condom before use, and coming into contact with semen before the condom is put on can all elevate the risk of infections. Thus, in-depth explanations are warranted to condom users to maximize their self-efficacy of use and to minimize their exposure to bodily fluids that could be carrying STIs (Duerr, 2011).
Treatment as Prevention
Recent findings have shown that Pre-Exposure Prophylaxis (PrEP), one of the newest HIV prevention strategies, is an effective tool that can be used to reduce the risk of HIV infection among men and women who are at high risk of becoming infected. Those undergoing PrEP treatment must take the pills consistently in order to maximize efficiency and effectiveness (Centers for Disease Control, 2013). However, PrEP alone cannot reduce acquisition of HIV. An intervention strategy that focuses on behavioral modifications such as an increase in condom use and a decrease in the number of sexual partners combined with PrEP may be the most effective way to prevent HIV transmission among high risk populations (Vissers, Voeten, Nagelkerke, Habbema, & De Vlas, 2008).
Limitations
The recommendations mentioned in this paper are a response to the condom riddle which only mentions one man engaging in sexual intercourse with three women. Yet, it is important to acknowledge that other vulnerable groups can also benefit from all of the mentioned strategies. A woman who engages in sexual intercourse with multiple partners and men who have sex with men (MSM) should also follow similar suggestions to reduce the acquisition of STIs and HIV transmission. Further discussions are needed to analyze the factors within these populations that may need an intervention to reduce the transmission and acquisition of STIs and HIV.
The public health implications surrounding the proposed solution to the condom riddle are important to examine in order to educate the public and develop new and effective strategies to reduce the risk of contracting STIs. The condom continues to be the most effective way for reducing these risks after abstinence. We must propose new solutions to the condom riddle that can educate the public on the importance of proper condom use, prevention of STIs, regular testing, reduction of lifetime sexual partners, and communication among partners.
Figure 1. Condom riddle posted solution
CDC. Pre-Exposure Prophylaxis (PrEP).Centers for Disease Control and Prevention (CDC), 19 August 2013. Available from: http://www.cdc.gov/hiv/prevention/research/prep/.
Condoms. Aids.org, (2013). Available at: http://www.aids.org/topics/aids-factsheets/aids-background-information/what-is-aids/safer-sex-guidelines/condoms/.
Crosby, R. A., DiClemente, R. J., Wingwood, G., Lang, D., Harrington, K. F. (2003) Value of Consistent Condom Use: A Study of Sexually Transmitted Disease Prevention Among African America Adolescent Females. American Journal of Public Health, 93, (6): 901-902.
D’Anna, L. H., Korosteleva, O., Waner, L., Douglas, J. P., Sindy, M.C., McIlvane, E., Malotte, C. K. (2012). Sexually Transmitted Diseases. 39 (9): 687-693.
Duerr, A., Gallo, M., Warner, L., Jamieson, D., Kulczycki, A., Maurizio, M. (2011). Assessing Male Condom Failure and Incorrect Use. Sexually Transmitted Diseases. 38(7): 580-87
Fitch, J. T., Stine, C., Hager, W. D., Mann, J., Adam, M.B., McIhaney, J. (2002) Condom Effectiveness: Factors That Influence Risk Reduction. Sexually Transmitted Diseases. 29(12):811-817.
Fontanet, A.L., Saba. J., Chandelying, V., Sakondhavat, C., Bhiraleus, P., Rugpao, S., Chongsomchai, C., Kiriwat, O., Tovanabutra, S., Dally, L., Lange, J. M., Rojanapithayakorn, W. (1998) "Protection Against Sexually Transmitted Diseases by Granting Sex Workers in Thailand the Choice of Using the Male or Female Condom: Results from a Randomized Controlled Trial," AIDS 12, no. 14 1851-59.
Greenwald, J.L., Burstein,G.R., Pincus, J., Branson, B. (2006). A Rapid Review of Rapid HIV Antibody Tests. Sexually Transmitted Diseases. 8: 125-131.
Himes, N.E. (1934) “Medical history of contraception”, New England Journal of Medicine, 210: 576-581.
Hollander, D. Failure Rates of Male and Female Condoms Fall with Use. (2005). International Family Planning Perspectives. 31(2).
Kolman, M., DeCoster, M., Proeschold, B., Rae, J., Ankeny, H., Genevieve, B.J., Sena, A.C. (2011). The Increasing Impact of Human Immunodeficiency Virus Infections, Sexually Transmitted Diseases, and Viral Hepatitis in Durham County, North Carolina: A Call for Coordinated and Integrated Services. North Carolina Medical Journal. 72(6): 439-446.
Lenstra, J. K., Rinnooy Kan, A. H. G., Boas van Emde, P. (1976) (1978) Interfaces between computer science and operations research: proceedings of a symposium held at the Mathematisch Centrum, Amsterdam. September 7-10, Mathematisch Centrum.
Lewis, M. (2000). A Brief history of condoms. In: Adrian Mindel,ed. Condoms. British Medical Journal Books
Macaluso, M., Demand, M., Artz, L., Fleenor, M., Robey, L., Kelaghan, J., Cabral, R., Hook, E. W. (2000). Female condom use among women at high risk of sexually transmitted disease. Fam Plann Perspect. 32:138–144.
MOH. “What care should be taken to ensure correct male condom use?” (2013). Department of STD, AIDS, and Viral Hepatitis. Ministry of Health – Brazil. Available at: http://www.aids.gov.br/en/pagina/faq.
Moran, J.S., Harlan,R.J., Thomas, A.P., Stone, K.M. (1990) "Increase in condom Sales following AIDS Education and Publicity, United States." American Journal of Public Health, 80: 607-08.
Origami. About the Company. Origami: condoms re-invented. (2013). Available at: http://www.origamicondoms.com/#!about/cwvh.
Ortiz, A. P., Marievelisse, S., Suarez, E., Santos-Ortiz, M. D.C., Tortolero-Luna, G., Perez, C.M. (2011) "Sexual Behaviors among Adults in Puerto Rico: A Population-Based Study." The Journal of Sexual Medicine 8.9 2439-449.
Packel, L. A., Dow, W. H., de Walque, D., Nathan, R., Mtenga, S. Evolving Strategies, Opportunistic Implementation: HIV Risk Reduction in the Context of an Incentive-Based HIV Prevention Intervention. (2012) PLOS ONE. 7(8) | e44058. Available at: http://www.plosone.org/article/info%3Adoi%2F10.1371%2Fjournal.pone.0044058
Potter, WD, de Villemeur, M. (2003) Clinical breakage, slippage, and acceptability of a new commercial polyurethane condom: a randomized, controlled study. Contraception. 68 (1): 39-45.
Secker and Warburg and Dingwall E.J. Early contraceptive sheaths, (1953) British Medical Journal, 1-40.
UC Berkeley. Two condoms, three women. Open Computing Facility (OCF) at the University of California, Berkeley. (2004). Available at: http://www.ocf.berkeley.edu/~wwu/cgi-bin/yabb/YaBB.cgi?board=riddles_easy;action=display;num=1129750094.
United States Food and Drug Administration. Durex Synthetic Polyisoprene Male Condom. (2008, June 19). Available at: http://www.accessdata.fda.gov/cdrh_docs/pdf7/K072169.pdf.
United States Food and Drug Administration. Condoms: Barriers of Bad News. (2009) Available at: http://www.fda.gov/ForConsumers/ByAudience/ForPatient Advocates/HIVandAIDSActivities/ucm126370.htm.
UNFPA. Male Latex Condom: Specification, Prequalification and Guidelines for Procurement, (2010). Geneva, Switzerland: World Health Organization, United Nations Population Fund (UNFPA) and Family Health International. Department of Reproductive Health and Research. 2013.
Vardi, I. (1991) Computation Recreations in Mathematica. Addison-Wesley Professional.
Vardi, I. (1993) Re: condoms. Email. Stanford University. 1993. Available at: http://www.mathematik.uni-bielefeld.de/~sillke/PUZZLES/condoms-n-m.
Vissers, D.C. J., Voeten, H. A. C. M., Nagelkerke, N. J. D., Habbema, D. F., De Vlas, S. J. (2008) "The Impact of Pre-Exposure Prophylaxis (PrEP) on HIV Epidemics in Africa and India: A Simulation Study." Ed. Gary Maartens. PLoS ONE 3.5: E2077.